Indian Scientists have suggested that large scale measures like developing pollen forecast systems and training of health care professionals and personal measures like following pollen forecasts, use of face masks, spectacles, and air filters, regularly taking prescribed medications, limiting outdoor exposure, and avoiding gardening or grass-cutting during peak pollen seasons could help minimize the onset and exacerbation of pollen-related allergic diseases.
They have highlighted the need for dissemination of proper knowledge regarding pollen allergy, allergen avoidance, their symptoms, and management to better address the ailment. Spring is in full bloom as the weather changes, trees, grasses, and weeds release fine bioaerosol particles known as pollen to fertilize other similar plants. However, pollen entering the nasal pathways could cause pollen allergy—with symptoms somewhat similar to common flu and cold. As the climatic variability is increasing, it is expected that the urban environment will significantly add to the burden of pollen-related respiratory and skin diseases.
Considering this, Prof. Ravindra Khaiwal from Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, Ms. Akshi Goyal, Ph.D. research scholar, and Dr. Suman Mor, Chairperson, Department of Environment Studies, systematically examined the implementation gaps to minimize the pollen allergy disease and suffering. Their study, supported by the Department of Science and Technology (DST), Govt of India, was just published in the International Journal of Hygiene and Environmental Health (IJHEH), an international journal by Elsevier.
The study aimed to understand the major causes of widespread pollen allergy and identify the implementation gaps to suggest key adaptive measures to minimize the onset and exacerbation of pollen-related allergic diseases, focusing on lower and middle-income countries.
“These submicronic-pollen particles could act as respirable particles reaching deeper into the upper airways leading to exacerbation of asthma, chronic obstructive pulmonary disease (COPD) and other allergic reactions,” Prof. Ravindra Khaiwal pointed out. He added that pollen allergy is a major respiratory illness that causes morbidity and affects patients’ quality of life. Over the past few decades, the prevalence of pollen allergy has increased. It affects about 10%–30% of adults and 20%–25% of children worldwide and has increased owing to urbanization, air pollution, and climate change.
Dr. Suman Mor, Chairperson, Department of Environment Studies, Panjab University, Chandigarh, highlighted the four levels of strategies suggested by them– individual level, health care communities and organizations, Local Governments, National/International Governments levels, to decrease the risk of illnesses associated with pollen allergy.
Prof. Khaiwal added that attention needs to be given to the most vulnerable sub-populations with allergic asthma, rhinitis, and eczema during the peak pollen season. He stressed that multi-stakeholder engagement is the key to minimizing pollen allergy’s impact, including focusing on the education sector to build capacity in aerobiological research, developing pollen forecast systems, and training of health care professionals.
Ms. Akshi Goyal, DST-INSPIRE Ph.D. Scholar, Panjab University, Chandigarh, said that the research provided her an opportunity to understand the severity of the pollen allergy in changing climate, and studies like these would encourage young scientists to build a career in the area of aerobiology to reduce preventable health risks.
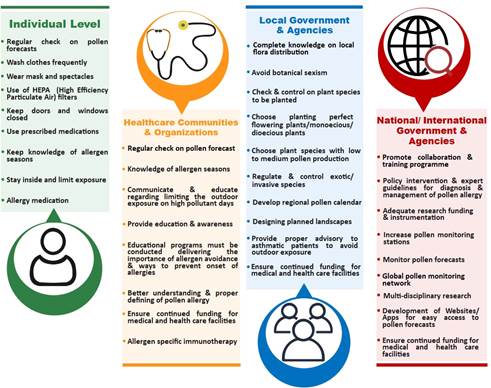
Figure: Key measures and recommendations for preventing and controlling pollen allergy.
 Indian Industry Plus A Pratisrutiplus Suppliment
Indian Industry Plus A Pratisrutiplus Suppliment